Blog
Beating the sneeze – combating hay fever
 Ugh. Runny nose. Itchy eyes. A brain fog that even a double-shot espresso struggles to budge. Hello, hay fever!
Ugh. Runny nose. Itchy eyes. A brain fog that even a double-shot espresso struggles to budge. Hello, hay fever!
Spring has sprung, my friends – and with it a generous hit of a billion teeny ants crawling inside your head! Well, at least for many of us.
If you don’t suffer from it yourself, it is likely you will know at least a couple of people who do. Hay fever (a.k.a Allergic Rhinitis) is a condition plaguing at least 1 in 7 Australians and is becoming more common.
There are several reasons as to why someone may experience an allergic flare-up, often due to inhalation of dust, pollen, mould, animal hair or other environmental allergens.
It can be seen alongside eczema, asthma, depression and migraine, and you may be more susceptible if other family members suffer from it, and depending on the state of your microbiome.
And there are foods.
Some foods contribute to the exacerbation of symptoms, especially those that enhance inflammation in the body. Yet some foods can offer resilience and respite!
Here are the ‘CliffsNotes’ tips for foods to limit, and foods to get in your belly.
Foods to limit
Refined sugar, preservatives, and heavily processed foods: Devoid of nutrients, possibly toxic, and wreaking havoc on energy levels, the gut and the immune system makes highly refined and processed foods lame. Avoid where possible, choosing the whole food version instead.
Gluten: There is a general anti-gluten tirade on trend at the moment. This protein found in grains such as wheat, barley, and rye is typically consumed in high quantities in a Western diet, largely due to many gluten-containing foods being highly processed. This means the gluten to everything-else-in-the-grain ratio is high; so overall, we may be exposed to more of the protein.
The issue? Gluten contains a class of protein called gliadin which has an effect on protective barriers in our gut, temporarily allowing stuff from our intestine into our bloodstream that really shouldn’t be there (a.k.a leaky gut).1
This may cause the immune system to lose its defensive mind, and encourage some of us to become more hypersensitive. So if you are going to have it, know that a little gluten exposure is okay for most, so long as it is eaten within a nutrient-dense whole grain and not its nasty refined, white cousin.
Alcohol: Now, don’t get me wrong. If alcohol agrees with you, a wee tipple can be fine. Simply consider that alcohol burdens the liver and the gut, and affects sleep. Therefore immune function may be compromised, which can contribute to increased susceptibility to allergic symptoms, and illness in general.
Dairy: It can make you snottier. Boo.
Foods to embrace
Boosting immune function and anti-inflammatory activity are important in building resilience to factors causing hay fever.
Overall, whole foods are your kick-ass arsenal equipped to support the immune system to respond appropriately to allergens. Here are some key nutrients and foods that may help:2;3
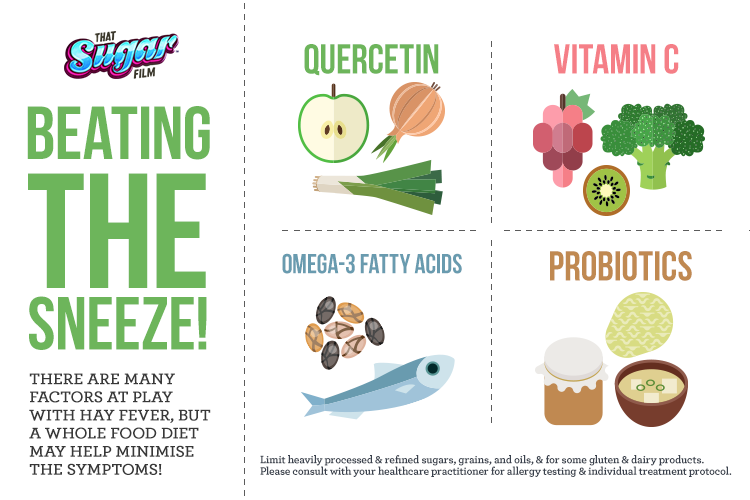
Quercetin: Foods like onions, garlic, leek, buckwheat and apples (with the skins on!) are filled to the with brim with the phytochemical Quercetin, an anti-histamine ninja.
Vitamin C: Tuck into berries, kiwi fruit, capsicum, dark leafy greens, and broccoli, as boosting vitamin C can inhibit histamine secretion from immune cells.
Omega-3 fatty acids: One study found higher levels of the powerful anti-inflammatory omega-3 fatty acids – found in oily fish, chia, flaxseed and leafy greens – was associated with decreased risk of allergic rhinitis.4
Probiotics: Local and systemic immunity can be supported through health and integrity of the microbiome. Enjoy prebiotic and probiotic rich foods, including a variety of sources of fibre and fermented foods such as sauerkraut, kombucha, and good quality miso.
Not mentioned in the graphic above, but also good to consider is zinc. The ultimate of immune supporting minerals, zinc can be found in sunflower and pumpkin seeds, spinach, beans, cashew, chicken, and cacao.
Diet helps, but it ain’t all
There are a myriad of lifestyle factors to consider too!
If you can identify external triggers, like dust, mould, or a particular tree that blossoms and sends your nose a-running, see what you can do to limit your exposure. Tips to tackle hayfever include:
- Using vaporisers to inhale helpful essential oils, such as peppermint, eucalyptus, and tea tree.
- Keep doors and windows closed up on windy days and days of high pollen count.
- Do not dry linen and clothes outside on days with high pollen count.
- Use dust mite covers on pillows and mattress.
- Undertake gentle saline washes with a neti pot, or nasal spray.
- Ensure you have adequate rest and daily exercise.
Read more on causes and treatments here and here.
Beating the sneeze over time
Considering over 70% of the immune system resides in our gut(!) building immune resilience through diet, and tending to your helpful gut bugs and the health of your intestinal microbiome, can help.
You may wish to consider being tested for environmental and food allergies, and food intolerance, as these can trigger and exacerbate symptoms. And there are plenty of alternative treatments too, such as herbal medicine and acupuncture. Check in with your trusted healthcare practitioner for further advice.
Overall, cutting back on unhelpful foods, and filling a majority of your diet with supportive vegetable and fruit will help. However, don’t expect an overnight miracle. Boosting immune resilience needs time.
But in the meantime, eating more fruit and veg can only be amazing for you, right? Right. 🙂
By Angela Johnson (BHSc Nut. Med.)
References:
- Fasano, A, Not, T, Wang, W, Uzzau, S, Berti, I, Tommasini, A, & Goldblum, SE 2000, ‘Zonulin, a newly discovered modulator of intestinal permeability, and its expression in coeliac disease’, Lancet, vol. 355, no. 9214, pp. 1518-1519.
- Hechtman, L 2012, Clinical Naturopathic Medicine, Churchill Livingstone, Chatswood, N.S.W
- University of Maryland Medical Center 2015, Allergic Rhinitis, viewed 15 August 2016, <http://umm.edu/health/medical/altmed/condition/allergic-rhinitis>
- Hoff, S, Seiler, H, Heinrich, J, Kompauer, I, Nieters, A, Becker, N, Nagel, G, Gedrich, K, Karg, G, Wolfram, G, & Linseisen, J 2005, ‘Allergic sensitisation and allergic rhinitis are associated with n-3 polyunsaturated fatty acids in the diet and in red blood cell membranes’, European Journal Of Clinical Nutrition, vol. 59, no. 9, pp. 1071-1080.